| Louis Quatorze:Feline | |
|---|---|
| Male Siamese, Seal point | |
| Born | Jul-1997 |
| Dx | Sept-2006 |
| Oral meds | : |
| Regulated | Feb-2007 |
|
Regulated between 50 and 120 | |
|
{{{regcomment}}} | |
| Remission | - |
| Insulin | Lantus, plus occasional booster of Regular |
Louis is a neutered male Siamese cat who was diagnosed with diabetes at age 9 in autumn of 2006, and started twice-daily injections of Lantus. Regulation was very difficult at first and took about 5 months, a switch to all low carb wet food, and a very high dose before he suddenly responded and the insulin dose had to be quickly lowered . He went into remission/ became diet controlled, 3 months after the “breakthrough” and 8 months since starting on Lantus. He was off exogenous insulin for a year, until in June 2008 he became extremely ill with pancreatitis and ketoacidosis. He has been back on Lantus since then and the majority of that time tightly regulated in a euglycemic range except for during occasional pancreatitis flare-ups. In 10/2009, after another such pancreatitis episode, he continued to have hyperglycemia, in what seemed to be a repeat of the insulin resistance in 2006, and it again took gradually raising the dose to a high level before he responded.
Background, symptoms and diagnosis[]
Louis had basically been healthy except for an upper respiratory infection when he first came from rescue in 1999, and an episode in 2001 of urinary tract infection and urethral blockage caused by struvite crystals. To prevent more crystals he was on a diet of Hills CD dry kibble, and over five years, his weight nearly doubled from 9 lbs (4 kg) to 16.9 lbs (nearly 8 kg). He did not have hyperglycemia in bloodwork prior to a dental prophylaxis in July 2006, but developed it sometime shortly after that. I do not know that there was a connection, but perhaps stress from the procedure added to some unrecognized problem such as chronic pancreatitis, plus the effect of being constantly bombarded with carbs.
Initially I noticed he was somewhat lethargic, spending most of his time lying on the floor in front of a fan, but I thought it was due to the hot weather. There began an insidious onset of polyuria, polydipsia and polyphagia with weight loss, until they became marked enough to notice. He also had some relatively minor neuropathy, although at that time I did not at the time know what it was. I noticed that he was avoiding high jumps, I saw that he fell/nearly fell when he attempted to jump; he also seemed less sure-footed on narrow places, stumbling in a way he had never done before, and seemed to walk a bit stiffly.
Louis was diagnosed in September 2006, and his blood glucose level was over 700 mg/dl! Possibly stress raised BG somewhat extra at the clinic but clearly this was a cat with raging diabetes, which was confirmed by fructosamine test. Fortunately he tested negative for ketones at that time.
Treatment[]
After the diabetes DX, before starting insulin, we first adding some Purina DM, (both dry and cans, but mostly dry) to his dry Hills C/D which made no dent in his diabetes, so he began Lantus /insulin glargine, initially at 2 units SID (once daily). 2 weeks later he went for a curve and BG still in 500s. Increased Lantus to 2 units BID (twice a day), which again made little difference in clinical signs of hyperglycemia. The dose was increased gradually with at least two weeks between each dose change. I had to began to read about feline nutritional needs, learned that more protein and less carb would naturally tend to acidify the urine and he did not need to be eating "prescription" food with chemical acidifiers. By December 2006 I had transitioned him to a low carb wet diet. (Incidentally, crystals have never again been found in urinalysis after he got off the high carb dry food.) With the diet change and raising dose to 8 BID he started to show some slight improvement but still in 300s-400s in his curve at the vet.
Overcoming glucose toxicity[]
By February 2007 we had raised the Lantus dose to 10 BID and suddenly the PU/PD decreased, Louis was no longer so hungry and thirsty, seemed to feel much better. From what I later read it seems likely that this was breaking through what the pet diabetes wiki article on glucose toxicity calls a "glass floor" of insulin resistance due to glucose toxicity. Unfortunately, having been discouraged by 3 vets, I was not yet hometesting blood glucose, which would have given me a better understanding of what was happening and would have been much safer: I did not know at that time that after breaking through that "glass floor", insulin needs rapidly drop. When I took him for his next appointment his BG was only 3. Within several weeks his dose went down all the way from 10 to 2, with BG and clinical signs showing a huge improvement from when he was on that same dose in 2006. I also saw an improvement in the neuropathy and he totally recovered from it. (I had started in December 2006 giving Methyl B-12 and that probably helped combined with the lower BG.) In the meantime I finally succeeded in testing his blood glucose at home which was essential to being able to keep him tightly regulated as his pancreas healed and took over more of the work.
Dealing with the “sputtering” pancreas: using food to lower BG![]
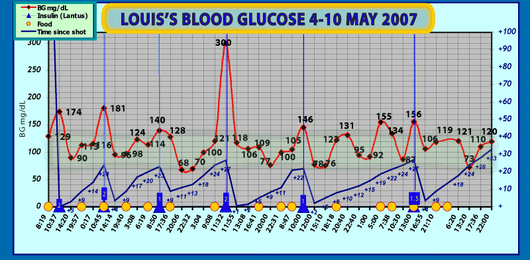
Chart 2: Louis's blood glucose levels in early May 2007, showing pancreas working part time. For the first few days, the BG level is in a more expected diabetic-type relation with the SID insulin. Then we see more ups and downs in the middle of a shot cycle as Louis's pancreas now produces insulin to lower BG in response to food intake. Note: Lower line (dark blue) represents hours post shot. Green band shows normoglycemic level. Click for larger high res image.
We made one premature attempt at stopping the insulin but after a couple days his BG started rising again (and some credit for those first two days may be attributed to the carryover effect of Lantus' insulin depot. Therefore we resumed Lantus, attempting tight regulation and shooting as needed, which became mostly SID as he got increased duration. Continued monitoring of BG showed highs coming down (aside from one shocking 300 (possibly insulin not catching up to a food spike or his pancreas fell back asleep for awhile) But one could see that at least some of the time he appeared to be lowering postprandial BG on his own. I began to divide Louis's food into multiple (about 6) small meals per day, to stimulate the pancreas without hitting it with too much glucose at once. Louis was getting definite postprandial drops in blood glucose so I could use food along with exogenous insulin as a tool to get his pancreas to bring DOWN blood glucose. In fact, food became the primary tool with Lantus as the back-up. I would test, feed and re-test about 3 hours later (this varies by cat); if BG had not gone down, I would then give exogenous insulin.
Remission June 2007-June 2008[]
This method proved successful and throughout the rest of May and early June 2007 Louis continued to get increasingly better duration on Lantus and to show evidence of a working pancreas. He went off insulin June 10, 2007. Louis did briefly have some higher BGs (mid to upper 100s) in late summer/ early autumn 2007 after he had gotten into high carb food. (it is also possible he had a minor pancreatitis episode; he had not yet been diagnosed and the signs can be subtle) I also noticed while he was off insulin that not sticking to the multiple small meals, or going many hours through the day with no food caused his BG to rise.
Louis survives Pancreatitis, Ketoacidosis, Liver Damage and UTI[]
In June 2008, after being off exogenous insulin for a year, Louis developed pancreatitis but at first showed no obvious symptoms. Unfortunately, since Louis's BG was no longer being tested frequently, we missed seeing the hyperglycemia that would have signaled that something was going very wrong. Glucosuria led to a urinary tract infection, also initially undiagnosed. The combination of insulin resistance due to inflammation/ infection and a somewhat lowered appetite put him at risk for ketosis, and when he stopped eating for a day he quickly spiraled into diabetic ketoacidosis. He was vomiting, lethargic, laterally recumbent, breathing in "sighs". I took him to the vet who took a look at him, ran some quick tests and found he was ketotic, his electrolytes were all out of whack, liver values screwed up and various other abnormalities, plus infection. She recommended immediate transfer to a 24-hour emergency / specialty animal hospital able to cope with a cat in such a critical condition. At the hospital it was pretty clear there was a good chance he would not make it until the next day. But he was not ready to check out. By the third day the vet called and sounded very happy. Louis was standing up and drinking water on his own, ketones were lower, electrolyte levels improved. He said "You've got a fighter" Of course he didnt fight on his own, it needed the excellent care he received there to save his life. Louis was hospitalized a week. Pancreatitis was diagnosed by ultrasound and by the fPLI test. The ultrasound also revealed diffuse hepatopathy. He was on an IV, Regular insulin, antibiotics and pain meds. They made adjustments based on frequent tests of electrolytes, BG etc. Basically they were doing everything as recommended in Dr Thomas Schermerhorn's paper Understanding Diabetic Ketoacidosis from the 2005 WSAVA congress, which I recommend that anyone whose pet has DKA read to help them understand and talk to the vet about the treatment. Pets CAN survive being as sick with DKA as Louis was, but for the best chance it requires prompt treatment of life-threatening problems, and close monitoring round the clock in a hospital, because things can change rapidly, and one aspect of the treatment can affect something else and levels of supplementation have to be adjusted.
Once the ketones were gone they switched him from R to Lantus again.
July 2008 – September 2010[]
In the first week or so after release from the hospital, Louis had erratic and often very high (400s to over 600) blood glucose levels, but this quickly resolved and within a few weeks after hospitalization, Louis was regulated. I followed the German Tight Regulation protocol for Lantus & Levemir (or at any rate the FDMB Lantus Group’s version of the same basic principles), and his BG was mostly 60-120. He was able to decrease his dose and got down to about 0.5 BID before another pancreatitis episode sent it up again. He has had a few such flare-ups but was able to be treated at home with medication and subcutaneous fluids, and sometimes needed temporary dose increases and boosters of R but was able afterward to get back to tight regulation and most of the time seemed to be feeling well. A few times he has had trace ketones in urine but has soon been able to flush them out.
Following his serious illness he was on Denamarin for his liver and within several months his liver-related blood levels were back in the normal range. He also had high creatinine levels in fall 2008, and at the time it was thought he was early CRI. But since then his creatinine lowered in the last two tests, from 2.8 to 1.8.
Glucose toxicity again rears its ugly head[]
But after a flare-up in October 2009, it was this time extremely difficult to get him re-regulated; his BG stayed high; In what seems like a repeat of the insulin resistance in his first months after diagnosis, the insulin dose was gradually increased from 2.5 to 8.5 units of Lantus BID by 2/2010 before he very suddenly started going into hypoglycemic levels - even under 20 - on doses that a few weeks before had left him in the 200s-400s mg/dL – possibly again broke through the "glass floor" of glucose toxicity, and this time I have the BG data to see how sudden and dramatic it was. At the time of this update, this has just happened and we are now of course decreasing his dose.
Some notes on diet[]
After quitting the Hills CD, I first was feeding Purina DM, both the dry and canned, then switched to Innova EVO--initially feeding both dry and canned Evo, but gradually transitioned to all canned. To give him a change I sometimes fed Wellness grain-free varieties. Later I began feeding mostly Merrick Cowboy Cookout or Surf and Turf due to the lower phosphorus and lower fat / higher protein. (I had heard pancreatitis might be affected by fat, and while I no longer think that is true in Louis's case, it still seems a better ratio to have more protein than fat.) But he still gets some Wellness, Evo, Nature's Variety and low-carb varieties of Fancy Feast, all under 7 percent carbs. If I need to slow BG drop or bring up BG I feed Merrick Grammys Pot Pie which is around 8 percent carb (but when it has been like under 30 I start with some high carb Fancy Feast, the grilled varieties.)